Introduction
The endothelium is the largest organ of our body, which is located in the vascular system and plays an important role in the protection of vascular hemostasis in many physiological and pathological events(1-4). The endothelium is a dynamic organ that can synthesize and release vasoconstrictor and vasodilator substances. When endothelial dysfunction occurs, the synthesis of factors such as nitric oxide (NO), which causes vasodilation, is impaired(5). Endothelial dysfunction plays an important role in the initial stage of atherosclerosis, atherosclerotic plaque growth, and development of thrombogenic events(6). Low-density lipoprotein (LDL) cholesterol levels are associated with the risk of cardiovascular disease and increase susceptibility to complications of atherosclerosis(7). Oxidized LDL inhibits endothelium-dependent vasodilation by disrupting the activity of NO synthase and causes endothelial dysfunction(8). High density lipoprotein (HDL) has been shown to increase the production of NO and endothelial NO synthase causing vascular dilatation directly and indirectly, and it has been shown to support endothelial cell migration and proliferation through different mechanisms(9-11). Literature information on the effects of HDL and LDL levels on vascular endothelial functions in patients with coronary artery disease (CAD) is partially insufficient. Therefore, in our study, we aimed to investigate the relationship between HDL/LDL ratios and endothelial functions in patients with CAD documented through coronary angiography (CAG).
Materials and Methods
Fifty-seven patients between the ages of 18 and 80 years, who had CAD documented through CAG, were included in the study. Patients who could not have a pulse from the radial artery, who could not have an optimal ultrasonographic evaluation, and who did not give informed consent were excluded from the study. In addition, patients with acute coronary syndrome and patients with normal coronary artery patency as a result of CAG were excluded from the analysis. Our study is a prospective, observational study. The clinical data of the patients were filled in the relevant places in the case report form. The medical treatment of the patients included in the study was arranged by the attending physician, and all patients were under optimal medical treatment in terms of CAD. Ethics committee approval of our study was obtained from Ege University Faculty of Medicine Clinical Research Ethics Committee on 26.12.2017 with the decision number 17-12.1/22. Written informed consent was obtained from all participants.
Flow Mediated Vasodilation Test
Endothelial functions were evaluated by using the flow mediated vasodilation (FMD) test. GE Healthcare Vivid E9 4D Cardiovascular Ultrasound System Device, 11L-D, 4.5-12 MHz probe was used for this test. The environment where the FMD test applied was quiet, at room temperature and bright. The FMD test was performed after eight hours of fasting, and patients had not consumed products such as caffeine, cigarettes, or tea that could affect the procedure. In FMD test, the arm cuff inflation till 220 mmHg lasted for 5 minutes for the occlusion of the distal hand or distal forearm arteries. Then, the cuff was deflation. As a result, endothelial factors such as NO was released, causing vasodilation in response to reactive hyperemia in distal and proximal vascular beds were provided. In order to measure the maximum artery diameter, the arterial diameter change was recorded by ultrasonographic method for 3 minutes after the cuff was deflated.
FMD percentage change was made by calculating the following formula;
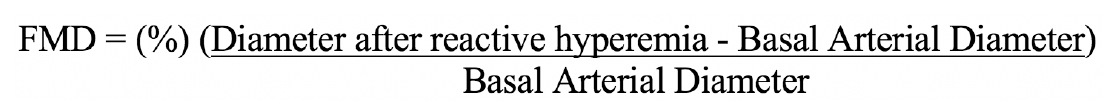
The radial artery diameter was measured in centimeters (cm) from the anterior wall intima to the posterior wall intima. Arterial diameter measurements were taken at the end of the diastole by determining the cardiac cycle with electrocardiography. The diameter and percentage change of the radial artery at baseline and after FMD were recorded.
Statistical Analysis
IBM SPSS Statistics 25.0 Program was used. The suitability of numerical variables to normal distribution was examined by using the Kolmogorv-Smirnov (n≥50) and Shapiro-Wilk (n<50) tests. Numerical variables were given as mean and standard deviation or median (minimum-maximum). Categorical variables were given as numbers and percentages. The Mann-Whitney U test was used because it was not suitable for normal distribution. The change in arterial diameter was examined with the paired sample t-test. The relationship between numerical variables was analyzed by using the Spearman correlation analysis. The significance level was accepted as <0.05 for all hypotheses.
Results
While the average age of 57 patients included in the study was 61.1±10.1 years, 70% of the patients were male and 30% were female. The mean body mass index was 27.8±5.7 kg/m2 and 57.9% of the patients were New York Heart Association (NYHA) class I, 42.1% were NYHA class II. The most common complaints of the patients were chest pain at a rate of 50.9% and dyspnea at a rate of 35.1%. The complaint of palpitations was present in 8.8% of the patients. 29.8% of the patients had a history of smoking and 19.3% had a history of alcohol use. The demographic characteristics of the study population are summarized in Table 1. Hypertension was the most common comorbid disease in 78.9% of patients. Apart from hypertension, the most common comorbidities were diabetes at a rate of 38.6% and hyperlipidemia at a rate of 33.3%, respectively. Five patients (8.8%) had chronic obstructive pulmonary disease and four patients (7%) had chronic kidney disease. Comorbid conditions of the patients included in the study are summarized in Table 2. Among the biochemical parameters, the mean urea value was 34.88 (±18.58), the mean HDL value was 44.88 (±10.86) mg/dL, the LDL value was 96.86 (±35.90) mg/dL, the mean hemoglobin value was 13.52 (±2.25) g/dL, and the mean fasting glucose value was 131.84 (±61.11) mg/dL. In echocardiography, the mean left ventricular ejection fraction value was 53.5±9.3%, the mean LV end-diastolic diameter was 4.87 (±0.56) cm, and the left atrium (LA) diameter was 3.9±0.6 cm. Laboratory and imaging findings of the patients are summarized in Table 3.
In the FMD test, the highest artery diameter was taken as basis in the measurements made during 3 minutes after hyperemia. The mean radial artery basal diameter was 0.25 (±0.029) cm, and the mean radial artery diameter after FMD was 0.28 (±0.033) cm (p<0.001). The mean radial artery percentage diameter change after FMD was 12.61% (±3.62). FMD test findings are summarized in Table 4, and the radial artery diameter change graph is shown in Figure 1.
The average HDL/LDL ratio of the patients included in the study was 0.53 (±0.26) and the median value was 0.42 (minimum 0.27 - maximum 1.50). There was a weak positive correlation between HDL/LDL ratios and the artery diameter percentage change that is showed as endothelial functions in FMD test (r =+0.379, p=0.04). The relationship between HDL/LDL ratios and FMD percentage change is shown in Figure 2.
Discussion
Atherosclerosis is a multifactorial disease caused by inflammatory, immunological and genetic events(6). Endothelial dysfunction is one of the main mechanisms in atherosclerotic process. Endothelial dysfunction not only plays a role in the first step of the atherosclerotic process that causes plaque formation, but also causes plaque to grow, cracking the plaque and trigger thrombogenic events(12). The endothelium produces NO, which inhibits the cellular pathways of inflammation, proliferation, and thrombosis(13,14). In normal endothelium, acetylcholine causes vasodilation and increases blood flow by stimulating NO release, while in the presence of endothelial dysfunction, it directly stimulates vascular smooth muscle cells and leads to vasoconstriction(1,13,14).
Vascular endothelial cell is the main target of pathological or mechanical injury caused by some risk factors such as smoking, increased systolic blood pressure, high total cholesterol, and low HDL cholesterol level(15). It has been observed that normal HDL taken from healthy subjects exhibits direct anti-atherogenic effects by modulating vascular endothelial functions(16-18). HDL stimulates endothelial NO production by activating endothelial NO synthase (eNOS), and also has antioxidant, anti-inflammatory and antithrombotic effects(19-22). We planned our study to evaluate the effect of HDL/LDL ratios on endothelial functions in patients with CAD under the same antithrombotic and anticoagulant treatment regimen.
Epidemiological studies have shown that HDL cholesterol has a protective effect against atherosclerosis, but the mechanism is not known exactly(23,24). Experimental animal studies have shown that HDL infusion acutely improves endothelial function(25,26). In vitro, HDL has been shown to protect endothelial cells against the damaging effects of LDL and to prevent oxidative modification of LDL particles(27).
The effects of HDL/LDL concentration ratios on vascular endothelial function in healthy individuals were evaluated on the basis of flow-mediated vasodilation response, which is a marker of endothelial function, and in our study, we found a weak positive correlation between HDL/LDL ratios and endothelial function.
In a study involving 26 patients who underwent routine diagnostic cardiac catheterization, it was found that high HDL levels improved intimal vasoconstriction in coronary arteries regardless of atherosclerotic wall thickness(28). Plasma HDL cholesterol concentration is a strong independent predictor of NO-induced peripheral vasodilation in patients with hyperlipidemia, diabetes mellitus, and CAD(29-31). As in animals, in individuals with hypercholesterolemia or low HDL, intravenous infusion of soluble HDL has been shown to improve the endothelium-dependent peripheral vasodilation by increasing NO bioavailability(32,33). Oxidized LDLs are a potent inducer of endothelial dysfunction. The protective effects of HDL on endothelial function are very important due to its capacity to resist the destructive effects of oxidized LDL(17,34). Low plasma HDL concentration is an independent predictor of endothelial dysfunction in healthy individuals and atherosclerotic patients(10). Our study confirms this information, and our study demonstrated that as HDL/LDL ratio increased, flow-mediated dilatation which evaluates endothelial function non-invasively, also increased.
Study Limitations
The single-center nature of our study is one of the limitations. The low number of patients may have reduced the power of the study. We believe that the strength of the weak correlation between HDL/LDL ratio and endothelial functions would increase if there were a higher number of patients. Another limitation of our study may be that endothelial functions were not evaluated by nitroglycerine mediated vasodilation test. The high ratio of male gender in the study may prevent the generalization of the study results over the population.
Conclusion
HDL/LDL ratio is related to endothelial functions in patients with CAD. As the HDL/LDL ratio increases, flow-mediated dilatation increases. We think that this study will be a pioneer to randomized studies that will be conducted on parameters affecting endothelial functions in patients with CAD.
Ethics
Ethics Committee Approval: Ethics committee approval of our study was obtained from EGE University Faculty of Medicine Clinical Research Ethics Committee on 26.12.2017 with the decision number 17-12.1/22.
Informed Consent: A signed informed consent form was obtained from the patients included in this study.
Peer-review: Externally peer-reviewed.
Authorship Contributions
Surgical and Medical Practices: M.K., M.A., Concept: E.S., M.A., Design: M.K., E.S., Data Collection or Processing: M.K., Analysis or Interpretation: M.K., E.S., Literature Search: M.K., M.A., Writing: M.K., E.S.
Conflict of Interest: The authors declared that there was no conflict of interest related to this article.
Financial Disclosure: The authors declared that this study received no financial support.