ABSTRACT
Surgical revascularization in patients with multi-vessel coronary artery disease still raises many questions.
The aim of the study was retrospective analysis of the single center immediate and mid-term results of off-pump Coronary artery bypass grafting (CABG) in patients with multivessel coronary artery disease.
This retrospective study includes 564 patients with IHD operated in the department of cardiac surgery in the Republican Research Center of Emergency Medicine in 2013-2017. Four hundred and seventy-three patients (84%) were male and 91(16%) were female, the average age was 56.2±0.9 years.
In the early postoperative period, 18 patients died, hospital mortality was 3.19%. Among the causes of mortality, there were perioperative myocardial infarction–eight (1.4%) and acute heart failure–eight (1.4%). In two cases (0.35%), the cause of death was septic complications. In a single-factor analysis, we observed that an unstable state on admission and emergent conversion to on-pump can be considered reliable risk factors for the development of the lethal outcome in the early postoperative period. During the follow-up period (2-40 months on average 24.1±0.34), 9 (2.4%) patients died, and the main causes of death were acute heart failure due to myocardial infarction in four (1.1%) and gastrointestinal bleeding in three (0.8%) patients. Freedom from the combined endpoint of cardiac death and myocardial infarction was 97.1% at 40 months; freedom from recurrent angina was 90.4% and freedom from repeated revascularization was 99.1%.
Patients with multivessel coronary disease and unstable angina in most cases can undergo off-pump CABG with favorable early results. Hemodynamical problems can force surgeon to turn on-pump. Emergent on pump conversion following hemodynamical instability can be a significant factor for mortality. In our series, CABG showed favorable immediate and mid-term results.
In this video, we are presenting a 36 years old woman applied with extreme cyanosis and short of breath followed with mis-diagnosis of a large interventricular septal defect (VSD) and pulmonary hypertension over the years. Having heard a loud and high-pitched pulmonary stenosis murmur on auscultation as a warning sign, the patient was referred to a pediatric cardiologist instead of her routine adult cardiologist. This time the echocardiography revealed a double outlet right ventricle (DORV) with extremely tight pulmonary stenosis and a large canal VSD which is commonly seen in such cases. We decided to close the large VSD with intracardiac tunnel patch and to supply pulmonary flow with a valved conduit as a Rastelli procedure(1-5). Due to the unavailability of a suitable sized valved conduit during the pandemic, we decided to tailor a custom-made valved conduit mounting size 25 SORIN biologic valve in a 28 mm JOTEC Coated Dacron graft.
The patient could take off cardiopulmonary bypass with positive inotropes and was discharged at two weeks postoperative. She is in New York Heart Association Functional Classification (NYHA) Class I status at fourth postoperative month after discharge.
Double outlet right ventricle is known as a connatural congenital heart disease in which both aorta and pulmonary trunk originate predominantly or entirely from the right ventricle with pulmonary outflow tract obstruction(6).
According to Anderson Classification both preoperative and preoperative assessments revealed as a Taussig Bing type of DORV associated with sub pulmonary VSD with transposition of great arteries(6-8).
After carefully echocardiographic and angiographic assessment of anatomy we decided biventricular repair with Rastelli procedure since both ventricles seemed as adequate size to reconstruct left ventricle outflow tract and right ventricle outflow tract properly(1,2,7,8).
Materials and Methods
This retrospective study included 564 patients with IHD operated in the department of cardiac surgery in the Republican Research Center of Emergency Medicine in 2013-2017. Four hundred and seventy three patients (84%) were male and 91(16%) female, the average age was 56.2±0.9 years. The initial patient data are shown in Table 1.
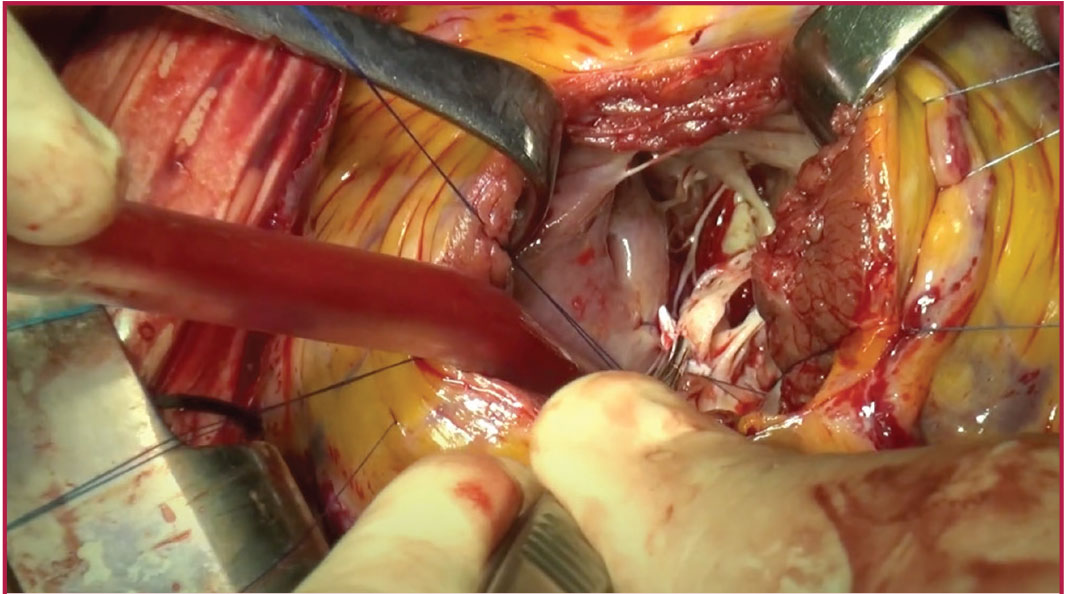
Most patients, 512 (90.7%), were operated; off-pump, standard deep pericardial stitches, Trandelenburg position, operating table rotations, volume preload and/or cardiotonic support were used to provide hemodynamic stability. During the procedure, we preferred to use the standard mechanical pressure stabilizer over vacuum stabilizers (Figure 1).
In most cases, (94.8%), the anterior artery was bypassed using the left internal thoracic artery, the mean number of grafted vessels was - 3.2. In 52 cases, we needed to turn on-pump due to several reasons. Of them, in 29 (5.1%) cases, the conversion was made urgently due to severe hemodynamical destabilization. Continuous variables were expressed as mean ± standard deviation and categorical variables as absolute numbers and percentages. Comparisons were performed with the two-tailed Student’s t-test for continuous variables and Fisher’s exact test, or χ2 test for categorical variables. All patients’ data used in research were used after the informed consent were obtained. Authors declared no ethical conflicts, and research was approved by the Ethical Committee of the Republican Research Center for Emergency Medicine (registered: 28.11.2018, REG no: 75). Authors declared no conflicts of interest or financial support from the third site.
Results
The immediate results of the hospital period, including hospital mortality and complications of the postoperative period, were evaluated.
In the early postoperative period, 18 patients died, hospital mortality was 3.19%. Among the causes of mortality, there were perioperative myocardial infarction-eight (44.45%) and acute heart failure-eight (44.45%). In two cases (11.1%), the cause of death was septic complications.
In a single-factor analysis, we observed that a history of acute myocardial infarction, diabetes mellitus, and COPD were not a risk factor for death, while an unstable state on admission [Odds ratio (OR)=15.38, confidence interval (CI) =-4.86-48.6 p<0.0001] and conversion to on-pump for emergency indications (OR=30.25, CI=9.46 - 96.7, p˂0.0001) could be considered as reliable risk factors for the development of the lethal outcome in the early postoperative period, a low ejection fraction also showed a high probability of a mortality, but the changes were not statistically significant (OR=1.07, CI=0.44-2.57, p=0.88).
Complicated postoperative period was noted in 77 (13.6%) patients. The heart failure - requiring cardiac support was observed in 23 (4.1%) cases, heart rhythm disorders - in 38 (6.7%) cases. Postoperative bleeding was noted in 6 (1.06%) cases, wound conducted complications in seven cases (1.2%). Ischemic stroke was observed in three patients (0.5%).
The duration of hospital stay in the ICU after surgery was 2.4±0.5 days. The duration of the postoperative period in the clinic was 9.8±0.9 days.
Midterm Outcome
During the follow-up period (2-40 months on average 24.1±0.34), nine (2.4%) patients died, main causes of death were acute heart failure due to myocardial infarction four (1.1%) and gastrointestinal bleeding three (0.8%). Freedom from the combined endpoint of cardiac death and myocardial infarction was 97.1% at 40 months. Kaplan-Meier analysis showed that freedom from recurrent angina was 90.4%. Repeat revascularization was required only in two patients, one patient showed progression of atherosclerosis in native vessels and another showed distal graft stenosis treated effectively by percutaneous coronary intervention - freedom from repeated revascularization was 99.1%.
Discussion
Some recent studies and meta-analyses have proven the safety and effectiveness of off-pump coronary artery bypass (OPCAB) with favorable early outcomes and have described OPCAB as a safe alternative to conventional CABG, regarding to death rate and postoperative morbidity(2,8,9). Fukui et al.(10) have revealed that the number of distal anastomoses per patient (3.6±1.4) in their study was similar to that in the on-pump patients, and complete revascularization was achieved in 99.2% of patients. In the present study, the number of distal anastomoses per patient (3.6) was the same as in Fukui et al.(10) study. We can state that complete myocardial revascularization using an off-pump technique can be safely performed. Sabik et al. (11) in their work described the equivalent midterm outcomes after off-pump and on-pump CABG, 4-year survival after OPCAB was 87.5%. The results of the present study, with a 40-month survival rate and freedom from cardiac death of 97.1%±0.6%, are almost identical to those of previous studies. The reduction of graft patency can increase the need for repeat revascularization with time. Puskas et al.(12) revealed that graft patency in OPCAB patients was similar to that in conventional CABG patients at 30 days (99.0% vs 97.7%) and 1 year (93.6% vs 95.8%) after surgery. In the present study, 90,4% of patients complained on angina recurrence, but overall early graft patency rate was 99.1%, what is almost identical to their results. Recent studies have revealed that off-pump to on-pump conversion can be performed in 5-10% of all cases(13). The rate of performing OPCAB in our isolated CABG patients was 90,8% and overall conversion rate was 9,2% with 5.1% cases being converted urgently due to hemodynamical disturbances. Some studies have underlined that conversion can be an independent risk factor for mortality in early postoperative period(13,14). Our findings also support these data, mortality rate was higher among urgently converted patients.
In the four largest studies in which off-pump and on-pump CABG were compared - CORONARY (n=2,357 vs 2,337 on)(15); DOORS (n=450 vs 450 on)(16); GOPCABE (n=1271 off vs 1268 on)(17) and ROOBY (n=1.104 off vs 1099 on)(18) there were no significant differences in the incidence of mortality, myocardial infarction or stroke in the early postoperative period or within 30 days after surgery. In the CORONARY and GOPCABE studies, in the long-term period, there was a higher need for repeated revascularization(15,17). In the ROOBY trial - data showed the absence of a statistically significant difference in the frequency of repeated CABG rates(18). In conclusion, none of these large studies showed a difference in major clinical outcomes between the off-pump and on-pump CABG during a 30-day follow-up(15-18). A recent meta-analysis revealed the favorable outcomes of OPCAB(1,8,9), and concluded that OPCAB should be considered as a safe alternative to conventional CABG with respect to mortality risk. Thus, we suggest that OPCAB should be performed whenever possible in patients undergoing isolated CABG.
Study Limitations
The limitations of our clinical study are that the number of patients was small, and the length of clinical follow-up was relatively short. Another limitation is that this is a single-center and single-surgeon experience.
Conclusions
Patients with multivessel coronary disease and unstable angina in most cases can undergo off-pump CABG with favorable early results. Hemodynamical problems can force surgeon to turn on-pump. Emergent on pump conversion following hemodynamical instability can be a significant factor for mortality. In our series, CABG showed favorable immediate and mid-term results.